While Disc injuries are a common culprit in spine related health problems, its function is widely misunderstood.
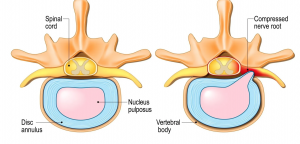
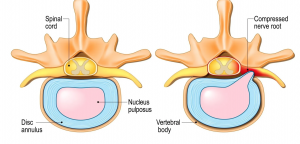
The (intervertebral disc) disc is a small cartilage pad that sits between most bones of the spine. The soft jelly like center is contained by surrounding layers of fibrous tissues. Each disc serves as a connector, space, and shock absorber for the spine. When healthy, discs allow for normal turning and bending without pain.
Since spinal discs have a very poor blood supply, they depend upon the circulation of joint fluids to bring in nutrients and expel waste when repairing from injury. If a spinal joint loses its normal motion or position and this pumping action is impaired, then the health of this disc can deteriorate. Like a wet sponge, a healthy disc is flexible. A dry sponge is hard, stiff and can crack easily. This is how many disc problems begin.
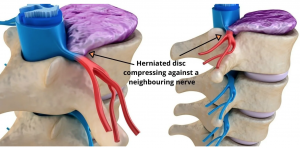
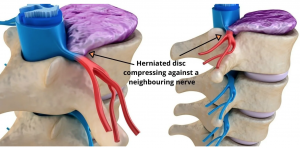
Because of the way each disc is attached to the vertebrae above and below of it, a disc cannot “slip” as commonly thought. However acute trauma and repetitive micro trauma (poor movement) can cause discs to bulge, herniate, or rupture. This can be quite painful, putting pressure on the spinal cord and nerve roots and on occasion send pain down the arms or legs, and cause muscle weakness.

These injuries walk through our doors frequently and patients can often be surprised at how effective the chiropractic management of these can be. The focused treatment approach of restoring better motion and position of the spinal joints will not only help decrease the inflammation and begin the process of healing it will also help de-load the involved disc.
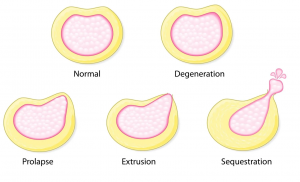
The following are all grades of disc injuries we treat at noth shore chiropractic Pymble:
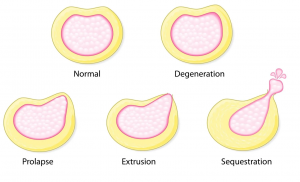
Disc Degeneration – The disc looses its fluid content and degenerates down to a rough, worn-out appearance.
Disc Prolapse – The disc jelly like material in the moddle of the disc pushes to one side, forward or backward and swelling occurs. It is however contained within the outer fibers of the disc.
Disc Prolapse – The most common disc injury, where there is a tear or microtears in the outer layers of the disc outside fibers with the jelly like material in the center pushing through.
Disc Sequestration – a piece of disc material seperates away and becomes a fragment or a free – floating piece.
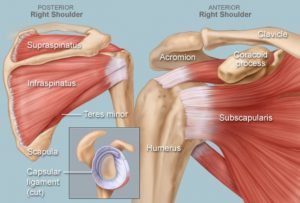
Rehabilitation (rehab) after a disc injury is crucial in strengthening up some of the surrounding muscles to the disc to limit the chance of re-injuring the weak disc.
If you would like to know if one of our experienced Chiropractors may be able to help you with your disc injury feel free to call and have a discussion with us – (02) 94407388